Meet Annie Morgan, a brave woman who underwent a bilateral styloidectomy to treat her rare and debilitating Eagle Syndrome. Though Annie’s journey to healing was full of hurdles, she found relief with CBD face cream and red light therapy, which she discusses in the episode. Tune in to learn about Annie’s remarkable road to recovery, and how cannabis has helped her manage chronic pain.
Table of Contents
Features
- Release Date: Wednesday April 26, 2023
- Episode Number: Season 1, Episode 10
- Special Guest: Annie Morgan
Listen To The Episode
Click the play button above to listen to the episode.
Listen to all podcast episodes →
Why You Will Love This Episode
Do you or someone you know struggling to cope with the horrible neck and ear pain caused by Eagle Syndrome?
Join this weeks guest, Annie Morgan, as she shares her powerful story of how she was able to heal from this debilitating condition.
In our conversation, Annie talks candidly about the emotional toll it took while battling chronic illness, why cannabis helped alleviate her symptoms, and other natural treatments that worked for her.
Through understanding the root cause of her eagle syndrome has been an integral factor in seeking treatment that truly works.
You’ll be inspired by hearing about just how much better life can be after facing down adversity.
Listen now to learn more about overcoming Eagle Syndrome with Annie!

Meet Our Special Guest
Annie Morgan is a true warrior and survivor.
Having been diagnosed in August 2021 with the rare Eagle Syndrome, Annie underwent surgery to correct calcified Stylohyoid ligaments that were severely compressing her Vagus nerve.
This debilitating illness had plagued her for almost 20 years, causing 33 different symptoms ranging from gagging and choking, high blood pressure, pounding heart, and significant gastrointestinal issues, to the sensation of butcher knives being stuck through her neck – among other things.
Bedridden for months leading up to her surgery, Annie had to endure the anxiety of five reschedules due to Covid-19 shutdowns.
With no guarantees of making it out alive, Annie’s story is a testament to the power of determination and resilience.
Despite it all, she emerged victorious and now shares her story of healing and the power of cannabis to help with chronic pain management.
Her journey inspires us all to keep pushing forward and never give up on our quest for good health and recovery.



What is Eagle Syndrome?
Eagle syndrome is a rare condition characterized by recurring pain in the back of the throat and behind the ear.
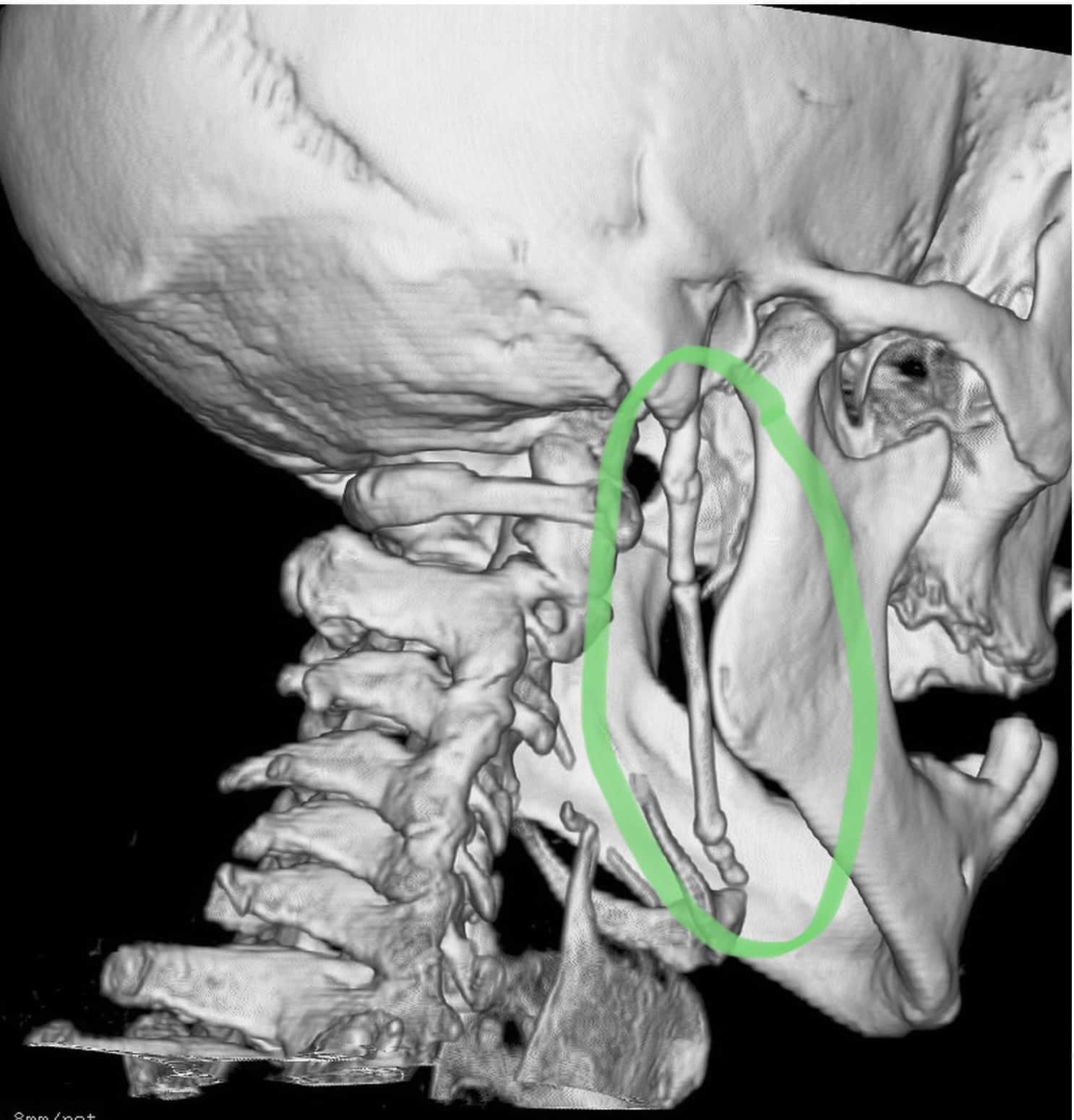
It is caused by an elongated styloid process, which is a bony projection at the base of the skull. When this bony projection is longer than usual, it can irritate the surrounding nerves and cause pain.
In some cases, Eagle syndrome can also cause difficulty swallowing or talking. Treatment options include pain management, medication, and surgery to remove the elongated styloid process.
Links & Helpful Resources
The helpful links and resources listed below will offer insight into the world of cannabis, providing knowledge and guidance if you are seeking answers on your cannabis journey.
Annie also want to mention that February is Rare Disease Awareness month (the month we recorded the show).
Eagle syndrome is an incredibly rare disease. For anyone out there suffering, Ben’s Friends – Living with ES is a wonderful resource.
Living with Eagle: Ben’s Friends is a wealth of information for patients struggling to deal with this syndrome,
The mission at Ben’s Friends is to ensure that patients living with rare diseases or chronic illnesses, as well as their caregivers, family, and friends, have a safe and supportive place to connect with others like them.
There is also an Eagle Syndrome Support group on Facebook.
Subscribe To The Show

Full Transcript
Announcer: Welcome to the Well With Cannabis Podcast, a show dedicated to telling the life-changing stories of those who live well with cannabis all while teaching you how to do the same. Meet your host, Emily Kyle, a registered dietitian nutritionist turned certified holistic cannabis practitioner. Emily changed her life for the better with the help of the cannabis plant, and now she’s committed to helping others do the same.
Tune in each week to hear heartwarming stories and gain the knowledge you need to feel connected, inspired, and supported on your own cannabis journey. Whether you’re a new cannabis consumer or a lifetime lover, you’ll benefit from these uplifting tales of real-life journeys that will show you how you, too, can live your best life well with cannabis.
Disclaimer: Hi there. Before we jump into today’s episode, I wanted to share a note on potentially sensitive content. The episodes on the Well With Cannabis Podcast are created for adult audiences only. We will, at times, cover sensitive topics, including but not limited to suicide, abuse, mental illness, sex, drugs, alcohol, psychedelics, and the obvious use of plant medicine. Explicit language may be used occasionally. Please refrain from watching or listening to the show if you’re likely to be offended or adversely impacted by any of these topics.
The information on this show is for informational and educational purposes only. It does not constitute medical advice. If any of the content on this podcast has brought up anything for you, please reach out or speak to a professional or someone you trust.
Emily: Hello and welcome back to another episode of the Well With Cannabis Podcast, and I am excited to be here today with Miss Annie Morgan, and I am so excited to connect with her on a more personal level, because I feel like I know Annie a little bit.
She has been a long-term, amazing customer of mine in the store, and she’s told me a little bit about her story, but today we’re going to get to hear it from her. So Annie, welcome. Thank you so much for joining me today.
Annie: Hi, Emily. Thank you for giving me this opportunity. This is exciting.
Emily: Oh, I’m so glad you’re doing this with me. You have quite the story. And so does it start in August, 2021 or does it start before then?
Annie: Technically it goes back almost 20 years. Because knowing what I know now, yeah, like that’s how far I track back the symptoms from this illness that I had. But yes, it was basically July of 2021, we were on vacation, and I woke up one morning with laryngitis, which we’re on vacation, and I’m talking, so I didn’t think much about it.
But at the end of August, I still had laryngitis, but by then I had started choking, gagging. It felt like somebody was sitting on my chest. I really thought I had pneumonia and went into urgent care clinics. And they were like, “there’s nothing wrong with you, you’re fine.”
I finally went to an ENT, took myself to an ENT and saw a PA who one time had a patient who described their symptoms exactly like mine, and she said, I remember her saying, “let’s do a CT scan and rule out eagle syndrome.” I’m like, “Eagle syndrome? What the heck is Eagle syndrome?” And then I came home and read about it and it was like, “oh my gosh, this is it.”
It was just like almost, I still can’t wrap my head around it sometimes, but Eagle syndrome is where the stilo-hyoid ligament in your neck, it comes off the back of your skull, right behind your ear, it calcifies, it hardens like bone.
I mean, never in a million years would I have ever, ever, ever imagined this or that it would cause all these crazy things in my body, but in my case, the angle that they were growing at and the thickness was compressing my vagus nerve. And your vagus nerve controls, I mean, from your feet to your head, controls everything in your body. And so it was basically shutting my body down one system at a time. Right?
Emily: For anyone listening, not looking, I’m speechless over here with my mouth open.
Annie: Yeah, no worries. I mean, it’s a crazy story to tell, but I feel like I have to tell it because it’s so rare. So rare. And so then it was finding a surgeon who believed me, somebody who would do the surgery, who believed my symptoms. There’s different kinds of eagle syndrome.
There’s vascular eagle syndrome where people have compression of the veins and arteries in their necks, and oh, it just causes horrible, horrible problems. People have what they call classic eagle syndrome that affects a trigeminal nerve, and they have more real severe ear and jaw pain that can’t be pinpointed to TMJ or other things.
But I think they need to have a category called Vagal Eagle for those of us who are affected with the vagus nerve, and I finally ended up with Dr. Trevor Hackman down at UNC Chapel Hill, I found him through a support group. These support groups have been amazing. They saved my life. And oh, Emily, oh my gosh, I can’t even believe this. This is so exciting. So, oh my God. It’s like, oh my gosh, I didn’t even think about this! So today’s February 15th. My surgery was a year ago, February 16th!
Emily: Oh my gosh, how full circle!
Annie: Oh my gosh, yeah. Oh my gosh, I didn’t even think it . Yeah, so it’s like, I was just going to say, the one year anniversary was coming up and I’m like, wait, it is the one year anniversary! It is! I didn’t realize it was just a year ago.
Emily: How did it go?
Annie: So he was able to, I went down and saw him December 9th, but everything was shut down because of COVID, and so my surgery was scheduled and canceled like five different times.
So I got my diagnosis the end of August, by the end of September, I was pretty much bedridden, like the symptoms, the nerve symptoms, this is what’s so hard to understand, and it’s so hard in this healing, and this is where you have been such a giant help to me. It’s so hard to explain, but the nerve sensations I had were like, it felt like somebody literally had their hands around my neck and they were strangling me. It felt like metal skewers were piercing my larynx.
It felt like I had literally, I could tell you the shape and angle of the knife, like big butcher knives, like going through my neck and up under my skull, high blood pressure, trouble breathing, I couldn’t tolerate heat, I moved into the guest room, the windows were wide open. It was maybe 40, between 40 and 50 pretty much all the time.
And it made me feel better, the cold, and now I understand that that affects the vagus nerve and it almost calms it. Insomnia, my bowels were shutting down, I had horrible gastrointestinal issues. Those are what tracked back 20 years that they could never quite diagnose.
Horrible abdominal pain, which I understand now is the vagus nerve that goes across your abdomen. I used to get these really weird flareups of pancreatitis. They could never understand why I got it, how I got it, but I had it like eight times. And so they knew something was wrong but it’s from this eagle syndrome.
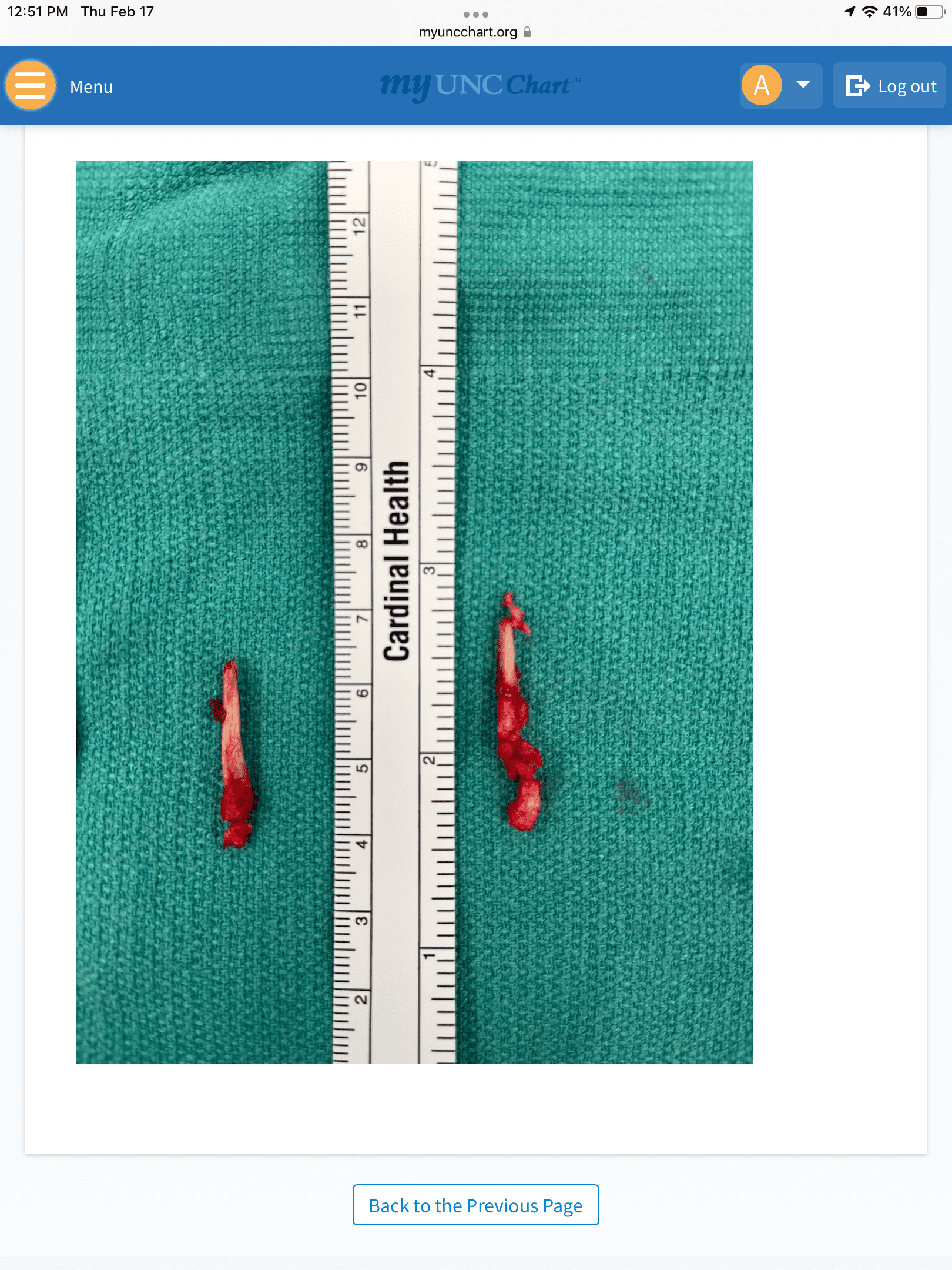
So anyways, I found Dr. Hackman, I had a bilateral styloidectomy February 16th, 2022. I can’t believe it’s 2023. And so they make an incision down the length of your ear, and then they make another incision in your neck here. And he did a great job. You can’t even see him. It’s in the crease of my neck, and so they clipped the styloid behind your ear, and they work through this incision in front of your ear.
They work around those structures, clip the styloid, and pull it out through here. So when they do that, you know, they open up your neck, they move all those muscles, all those nerves. So all these nerves are stretched. Those nerves were under really major compression. And in my case, Dr. Hackman said I was the worst case of vagus nerve compression he’s ever seen.
Yeah, I’m always like, go big or go home, right? Gah, I love that man. He’s amazing. Oh, yeah, he did my surgery and within 24 hours, I knew something significant had changed. Within 72 hours, my pain, I mean, pain that I had dealt with for almost 20 years was gone.
Like, still I’m just covered with goosebumps and I still have almost no words for it, but we stayed down in Chapel Hill for six days, I came home, had zero complications, zero complications, which is so rare for me. And for the first two weeks, I couldn’t hardly speak. I would get up in the morning and come out of my room. My husband, his desk is right outside that, our guest room there, and he’d be sitting at his desk and I’d come out and tears would be going down my cheeks and he’d, he’d just look at me, and go, “oh my gosh, what is wrong?”
And I’d just be like, “there’s just no pain. Like the symptoms are gone. I can breathe.” My blood pressure went back to normal immediately, immediately my pulse went back to normal. The pounding heart, it was just like all of those symptoms were just gone. But then, and the first one in two months were euphoric like that.
And then as everything started to calm down, it was like, “holy hell, what happened?” Because these nerves that were compressed for almost 20 years or longer, all of a sudden that compression’s gone. And so all of a sudden you’re sending all these signals that are, “oh, look here, everything’s great. Let’s do this now.”
But your body’s like, “wait, we have been sick. We’ve been working in this chronic stress mode. We’ve been sick. We don’t operate like that.” Like, “wait.” And then up here it’s like, “wait, we’re injured. We were stretched, we’re inflamed,” so you have like all these crazy signals going all these different directions and it’s exhausting.
Like I look good, I feel great, but inside my body there’s so much healing going on and it’s almost hard to manage. When I was in high school, I played fast pitch softball and I played first base and I played inside the baseline and I loved it, I loved it so much. And I took a batted ball to the face. I still remember how hot that ball was. I remember thinking, “this is hot.”
And the next thing you know, I was looking at the sky, but it knocked a tooth out on my upper left jaw here. It knocked a tooth out when I was 17 and I had root canals in these front four teeth. It did so much damage that in 2011 I had to have really major dental reconstructive work.
I lost six teeth here, and they had to, basically, it was a five year surgical process to rebuild my upper jaw bone, and it was skin grafting and bone grafting and placing implants. And it was a really long process, but I have beautiful teeth. But they think that it was possibly that injury that caused the eagle syndrome.
Yeah. And so anyway, so after surgery, I had some temporary facial paralysis, it resolved after about six months, but that’s where I found you. And I’m telling you, I had never used products like yours before, ever after a surgery or not ever to treat or heal from something like this. But I knew I did a lot. Like nobody tells you how to heal from the surgery, first of all.
Which is one of the reasons I’m going to start speaking about this, because people don’t understand. But I did a lot of reading about people who have palsy, Bell’s palsy, where they have sometimes their paralysis on one side of their face, stroke victims.
And a lot of it is massaging and real gentle massage. I knew that I didn’t want to stretch or pull on the nerves because they were healing. That’s where your face cream, oh my god, in fact, I use it, I should have it right here so I can show everyone. But this morning I woke up at like four and I have a face lighted mask and I use the red light therapy-
Emily: Right light? Excuse me, Oh my gosh. I want one so bad. I’ll have to ask you about that.
Annie: They’re amazing. I used to before my surgery and I really liked it, ’cause I think I have that seasonal effective, hate the winter. Whole other story. But anyways, I got up and did my 30 minute red light mask and then I do my face massage with your face cream.
And I like your face cream after surgery better than the recovery cream because it doesn’t have those heavy menthol or, you know, herbs in it, essential oils, which those are great for the muscular things, but around the incisions in your face, the face cream is amazing.
So as this is healed, like my facial was really tight, my lips curled up over my teeth. Like it was awful. I could have fork in my mouth, but I couldn’t open my mouth to take a bite, so it was months off, it’s still a little funky. It still feels a little bit-
Emily: I was just going to say like, you look so amazing, I can’t even believe that this was less than a year ago.
Annie: Oh, I mean six months ago, I finally could do…
Emily: Wow!
Annie: That was six months ago. That was like the last big thing I would do the, A, E, I, O, U, couldn’t, my mouth would not move like that. I couldn’t force it to. And so it was just like a giant Fu Manchu mustache, almost the tightness, how it pulled across and down.
I used your face cream and that CBD, when these nerves in my face flare up. Oh my gosh, it helps so much. I can’t, I wish I understood a little bit more about why, but it really-
Emily: So from my understanding, if you don’t mind me interjecting.
Annie: No, please do. Because it’s fascinating, ’cause it feels like, so people sort of understand as you explain this for me, if you’ve ever turned on an electric fence or how it just sort of hums and vibrates. That’s what the nerves underneath my skin feel like. It’s just like, it’s the healing energy. It’s so intense, it vibrates, and people who have experienced this will know. And so your cream, you tell me like, it’s amazing.
Emily: So not to be like too scientific, and I’m not like a hundred percent the expert. From my understanding, our skin has receptors, CB-1 receptors, CB-2 receptors.
And so when we apply CBD or THC or anything specifically on the skin, it interacts with the receptors exactly where you put it. And that’s why it provides the relief, because we have these receptors and it’s working.
And so I don’t know the exact mechanism of how it helps to reduce pain or tightness, but those receptors that are on our skin are what makes it work, which is so exciting to hear you’re having such success with the just CBD too.
Annie: Yeah, yeah. Just I sort of developed my own kind of massage that I do and every day it’s just been amazing. I have no scar tissue. I’ve been back to the ENT a couple of times, Cara, my angel, my darling angel Cara, the one that diagnosed it, and so she’s done a couple of my follow ups and she’s like, there’s not a smidge of scar tissue in there, so all that massaging, and again, it doesn’t pull the skin, it doesn’t pull on the nerves. It’s wonderful.
So brain fog was a really bad symptom, like, it’s so hard to explain. It’s like being hungover and drunk still at the same time. Like you can’t form a thought. You’re not coherent. You can’t put two and two together, and you’re like, you know you should be able to, but you just can’t. It’s bizarre. But that went away, but I used your focus product.
Emily: Yup the CBG?
Annie: The daytime, yeah. And I had never used, I really liked that. Now that I’m better, I don’t really need it, ’cause I feel that way naturally.
Emily: Uh, I’m so glad.
Annie: Yeah, but I liked it because what I’m learning is there’s so much to know about nerve memory, very much like muscle memory, but nerve memory, and how you have to retrain your nerves to learn how to live normally and learn how to live pain free and be happy and well, and so, you know, have a positive attitude.
You know, being outdoors, being in the sunshine, people are always like, blah, blah, blah. Well, there’s really so much to it. I mean, it’s all part of it. And so the CBD, the one with the CBG focus, the first couple months after, as I’m looking where I keep on my little goodies over there in the morning, just helped me like get back into a routine again and be like, “oh my God, this is what it’s like to get up.”
Like I was bedridden for four full months leading up to surgery. I mean I literally, you know, I could get up and go to the bathroom, I did a little bit of laundry, I would change the beds once a week. I did nothing beyond that. No, I had house cleaners coming, I couldn’t do anything beyond that.
And so my muscles were in an early state of muscle atrophy when I had my surgery, when my blood work came back, when I was in the hospital, they came in and said, :hey, so I’m doing a lot of supplements, a lot of work, a lot of counter fascial strain, cranial sacral work, lymphatic drainage, I use tuning forks to help the tinnitus and the nerves that are healing around my ears.
So I had 33 symptoms related. I listed every single symptom I had, and when I went to my consult with Dr. Hackman, I’m like, “I don’t know if these are all related, but here’s every single thing I’m feeling.” So 32 out of 33 of those symptoms resolved after surgery. Tonight, I know, right?
Emily: My gosh, congratulations.
Annie: Thank you. I still have no explanation for it. It’s a miracle to me. I feel like God granted me the most amazing gift of healing. That’s why I feel like I have to talk about this, because nobody talks about this healing part of it.
And had I not done the work I had done, I would not be as well as I am today. And I think it’s not just one thing, it’s a combination of all of them. But the last thing I’m going to tell you that is the hardest thing I’m dealing with right now, If you’ve never read about vagal health, vagal tone, there’s a lot to it as this vagus nerve is healing because it did live in a state of sickness for so long.
That’s how I refer to it in my healing terms. And so now that it’s getting well, it’s almost having a really hard time learning to be normal again. Sounds really crazy to say that, but some of the work that I go to for physical therapy is visceral work.
They do these, these releases on your abdominal area to help your organs work again. It’s crazy, it helps. But as the vagus nerve is helping them develop this anxiety, and I’ve never, never in my life, I mean everybody has nerves, whatever.
Emily: Interesting.
Annie: This is completely different. Completely different. And the first time we had friends coming over, friends we’ve had for 30 years, and I literally was in the bathroom crying, shaking, and they’re like out here in the kitchen and Brian comes in and he is like, “Annie, Brooks, and I are going to go play golf. Sherri’s in the kitchen, are you coming out?”
And I’m like, , and I was like, “what the hell is wrong with me? And I’m thinking, “this is anxiety.” Like I literally was having an anxiety attack. And so I’ve had three of them like that now I in the last couple months.
I’ve felt a little, I know it immediately, it’s like my nerves are so heightened as I’m healing, I feel I am like the princess and the pea, and I feel every little thing, but I feel the sensations of it starting. And so now I know immediately like, just breathe. You’re fine. Like, roll the window down for a minute, take your sunglasses off. Like there’s all these little tiny things, but I’m telling you, your products help.
Like, calm that down because, I don’t know, I don’t know any other way. It sort of takes you out of your own head so you don’t think about it as much. It takes the edge off that nerve sensation for me. I don’t know any other way to explain it, but-
Emily: I’m just so glad that you found something that can help and that you recognize that it’s coming, and so you can do like a little bit of preventative and just to take care of yourself when it happens.
Annie: Right. It’s really, it’s fascinating to me. And I’ll tell you a story that, you know, I think medicine is so tied into money, which is again, a whole other topic and pharmaceuticals and money and medicine, which is a whole other topic, but I think they love to write you a prescription and say, “here, go take this.”
They don’t want to get to the core of what your problem is. They don’t want to look for what the real answer is. Take the symptoms, go away, keep coming back, we’ll keep going, doing tests, keep giving you prescriptions, here’s more money, here’s whatever. You know the cycle. Anyways, right before my surgery, the guy who was my gastroenterologist who took care of me for 17 years, God bless the man, Dr. Scedera. And I have a really great story if we have time to tell you about him.
Emily: Yes.
Annie: Anyways, my gastroenterologist for 17 years always knew that there was something wrong with me. We could never quite figure it out. He never doubted me, always was willing to try new things, look at new things, whatever, always open to it, would come back from conferences and say, “hey, I heard about this. Let’s try this.” Love the man.
Well, he retired December 31st, so he’s the one who treated my pain, and so he’s the one that always wrote my prescription for pain medicine and things when I needed him. So since he retired, I had to find this new pain management doctor. So after 17 years at the worst health crisis of my life, I have to find this new doctor, right?
So I go in and he was a great guy and treated me and he was wonderful, but part of his clinic’s practice was doing a drug test. And so I had been taken CBN for sleep, like the nighttime one because I was only, I had really severe insomnia. Insomnia is a really bad side effect, and I was not sleeping more than maybe 45 minutes at night. Like it was horrible. It really truly was horrible.
I would not have lived another two months had I not had that surgery. Like it was bad. And so on the fourth visit, I went into him, third, fourth visit as I walk in, like they hand me a drug test and I take, you know, I just went in and did it, and he comes out, and he is like, “how are you doing?”
And I think at that point I had just started it and I said something to him, he is like, “how are you doing?” And I said, you know, “the sleep is killing me.” You know, I said, “I finally started taking this nighttime CBD, like I just, I have to sleep more. My body’s just dying. I can feel it, it’s dying.”
And I remember him saying sort of offhandedly, and again, I was so sick and I had that brain fog, I didn’t process things and I didn’t respond normally, but he said, “oh, you’re going to have to be careful with that.” He goes, “if you pop a positive,” he goes, “you can’t do both pain medicine and CBD.”
He said, “you’re going to have to make a choice between one or the other.” But he sort of said it like, that’s a scripted answer, what he says to everybody when they say blah, blah, blah. And I remember thinking, “are you for real?” Because it’s not one or the other.
Again, it’s not one of these modalities it’s helping me heal, it’s the totality of all of them that’s given me this result. And it was like, again, for me to talk about it, talk about using it and how it’s helped me, it was because that was the most freaking absurd thing to say. And it’s like they just don’t take into consideration how it helps.
Emily: I am always mind blown when I hear stories like this about the pain management clinics. I did not realize that they are like this, but apparently they all are, because you’re not the first person to tell me.
They’ve went to their pain management clinic and said, you know, a few test positive on a drug test, CBD, THC, whatever, cold turkey, you’re out the door, we don’t want to see you again. And I feel that the most inhumane, unacceptable answer, especially in pain management. It blows my mind that this happens to people. It’s not right.
Annie: Yeah, yeah, yeah.
Emily: Like why one or the other, I don’t understand why does it have to be one or the other? What if they both work together?
Annie: Yeah, the CBD at night was at least helping me rest in bed, because I was just laying there dying. I mean, I literally was in my bedroom with the door shut. I didn’t see anybody. I couldn’t talk, I wasn’t eating, I could maybe talk.
God bless my girlfriends, they know who they are, would call and chat with me, but you know, after probably 15, 20 minutes, I’d start coughing and choking to the point that then I’d start gagging, gagging would lead, then I would start throwing up, and it was just horrible. Nausea ,really, oh my God. I should have sent you my whole list of symptoms. ’cause you wouldn’t believe them- 33!
Really severe nausea was another really, I had those wristbands on 24/7. And again the CBD helped so much with that. Like, again, between the, oh geez, now I don’t remember, Zofran, I think the name of it was.
Between the wristband and the Zofran and Seven Up and CBD and cold air, you know, I could lay in bed and not move and not throw up all day. But without any one of those I would’ve been miserable. So it’s so unfair for them to say, “oh, you have to make a choice.”
Emily: Absolutely. And it’s just mean. I feel like it’s very mean on a human level to take somebody in pain and be like, “I don’t care what’s working for you, you’re going to do it my way or you’re not going to do it at all.”
Annie: Well, they don’t understand it. They don’t understand it and they don’t want to talk about it.
Emily: Have you had any doctors throughout this process that have been supportive of cannabis use?
Annie: I haven’t talked to any of them about it. Like, I didn’t, like at the time that I left, like my pain management guy after my surgery, I only saw him one time because I was literally pain free. Like I did not need to go back to him. And my surgeon, no.
Like I’ve just, and I think I’ve only talked to him a couple of times, but going forward and part of my healing, when I had my last appointment with Dr. Hartman in the end of September, I talked to him about some of this healing. I said, “I’m doing great. Like everything’s going really well. I said, I don’t really want to talk about me. Let’s talk about how we can help other people heal.”
And so as I’ve started pulling up all the research I did that helped me in putting it together and sending it to him, this is part of what I am and talk about. And I did talk about it in my last one I sent to him because it was about the massage.
And I said, I used a CBD cream, and it helped not only like prevent tugging on the skin, but when my nerves flare, and again, I know you guys can’t see it, but what I’ve learned is I’m not in pain, but like even my hands are eyes are ice cold right now and my face is really hot.
As my nerves are healing, this nerve energy, it feels like my face, like right here around my ears, this light little V here, and around my mouth, it feels like I’m sunburned really bad, really badly. And then I’m just radiating the heat that you do after a sunburn. And so this nerve heat is just another kind of nerve pain. And it’s just the healing.
And again, massaging it, that cream, just helps soothe it like nothing else. I use my little washer roller. I, you know, use my little ice pack periodically. I’ll put cold on it. So yeah, so I do, I have talked to ’em, started to talk to ’em about that. But yeah, more about the products and what they do, because again, this nerve healing, nobody talks to you about it, so.
Emily: And this whole story you’ve said is really shown me how important it is to be an advocate for yourself. You had to be an advocate for yourself. Not only to get a diagnosis, but then to feel well after the surgery. I’m really proud of you. And when I look at you, and I think that that was just a year ago, to see how well you’re doing now. Oh my gosh. I’m so happy for you.
Annie: Thank you. I mean, technically I should be a little further along. On the 4th of July, a chick driving a truck bigger than me rear-ended me, and luckily I was coming to a stop at a light and she had to be distracted, I was still moving, and she rear-ended me and it jarred everything.
And at the time, this was in July, about five months after surgery, and it set my healing back about three months. Didn’t cause any new injuries, but it jarred everything again, so all those nerves that were doing so well took a good hit. And so I should be a little bit further along, but it’s amazing. I’m just, I’m so blessed that, I mean, I have a very strong faith and I believe God has had a hand in this. I could tell you a hundred stories.
Let me tell you my little story about Dr. Scedera, ’cause it’s amazing really quickly. So he knew that I had this diagnosis and he retired December 31st, but my surgery wasn’t until February 16th, so he never knew my outcome. This man who stood beside me all those years, never doubted me, never questioned me, always fought for me, championed for me, took care of me, every day after my surgery, I thought about him.
Every single day, I thank God for him. Every day I put out into the universe how grateful I was that he was there for me because this was some real stuff, right? And so one day I’m out walking to my neighborhood while I’m healing, and this neighbor who lives behind me, Marilyn Nichols, were visiting out front and she’s like, “you’re looking great. Everything’s going good.” And I’m like, “yes, yes, it’s great.” But I said, “the one thing, I really just wish I could talk to Dr. Scedera.
He was my gastroenterologist. My heart just hurts that I haven’t been able to tell him.” And she’s like, “Scedera? We sold our house, you know, in the town they moved from to a gastroenterologist named Scedera,” you know? And I’m like, “oh my God, that was him.” So she gave me his address.
This was back in April. And so I’m like, yeah, whatever. So whatever. And so just went on and on. In September, I couldn’t stand it anymore. Finally, I’m like, “I have to let him know.” So I sat down and wrote him a letter. Told him about how I knew Marilyn and she gave me the address. I wasn’t stalking him. I said, “but you of all people needed to know how much you meant in my life and that you made a difference in my life. So happy retirement, you don’t need to contact me, my heart just needs you to know that you were important.”
And so, gosh, it was like the week before my birthday, the end of October, my birthday’s November 6th, so the week before my birthday, I get this card in the mail. And on the front of it, it said, “always believed something good was about to happen.” And it was from Dr. Scedera.
And he is like, “I’m so happy to hear your news.” He’s like, “that’s the best thing ever.” And he said, “leave it to you to track me down in retirement, you and your small world story.”
Emily: Oh my God, that is so beautiful.
Annie: Yeah.
Emily: It’s so nice to hear that there are doctors out there who fight for their patients, believe in their patients. And want the best for their patients. It’s so sweet.
Annie: And you have to thank, you have to let those ones know that you love them and that what they do makes a difference. Because it does. Yeah, yeah.
Emily: I was also thinking about, you mentioned your PA Cara, if she didn’t have that experience with Eagle syndrome, what if she never diagnosed you?
Annie: Oh my gosh, Emily, you’ll make me cry. Like I’ve belonged to a couple different support groups and Eagle syndrome and especially Eagle syndrome that affects your vocal chords is very rare. Even Dr. Hackman, who is one of the top doctors, he’s one of the only doctors who removes both of them at the same time. He’s just amazing.
But anyways, when I first saw him, when we talked about my laryngitis, he did this. He’s like, “that’s not related to your eagle syndrome.” He is like, “glossal pharyngeal neuralgia, we’ll send you to a specialist after surgery,” blah. Totally blew it off. But at the time, whatever.
But I knew it was from whatever was going on. And so had my consult with him, he said that. A few weeks later I was, ’cause I always research, I’m constantly reading, learning, trying to find out more. I came across this diagram which showed the lower branch of the superior laryngeal nerve goes right into the back of the larynx, and that branch is off the vagus nerve.
So if you have compression of the vagus nerve, it makes sense, right? So of course I threw my little MyChart account, sent him a picture of the diagram and say, just what I said to you basically, right? And he writes back and he is like, “Hmm, that’s really interesting. Thanks for sending that.”
He said, “but we’ll only know for sure if your symptoms resolve after surgery.” And so it did. And so my laryngitis resolved. You can hear I still get a little froggy when I talk too much, ’cause the nerves are still healing. But even he said now he attributes laryngitis as a symptom of eagle syndrome.
He said before he goes, “I never really had people who talked about it, but you were very obvious.” And so now they classify it as a symptom.
That’s amazing. I feel like through your whole story, now you’re kind of out here helping others. Talk a little bit about your newfound passion for helping others.
Oh my gosh. So this is not my comfort zone. Like my last job that I retired out of for health reasons because I was not doing well, but it was event planning, and I loved it because we worked with a lot of nonprofit, military nonprofits, Medal of Honor Foundation, Fisher House, Marine Corps Scholarship, disabled, I mean so many wonderful ones. I couldn’t even name them all, Fisher House, wonderful.
But you’d sort of swoop in, you’d do your event, you’re in the background, everything’s going on. It’s all wonderful, wipe your hands, go home, it’s all great, next event. So for me to be in the front talking, this is not my comfort zone, but I saw this TED talk with this young girl named Nora Sophie and she’s in Austria or Sweden, I think she’s in Sweden.
And her story was almost exactly like mine. She just woke up with laryngitis one morning and she couldn’t talk. But she was young. She was in her teens, late teens, 17, 18 when this happened. Went to probably 50 different specialists who did all these different treatments, but nothing for eagle syndrome. And so her vocals, she had so much damage in her neck and her vocals that she had a lot of permanent damage as a result of that. She didn’t get in her eagle diagnosis until later in her illness.
And she just recently had surgery to have her styloids removed. But anyways, she did a TED talk about it and somebody posted it, and again, I have goosebumps, somebody posted it, ’cause I love her in our eagle syndrome support group. And you listen to this young girl talk and tell her story, and it’s heartbreaking. It is absolutely heartbreaking.
I think the percentage that Dr. Hackman said, my risk of getting this is like 0.0012. That’s how rare this is. So February is rare disease awareness month. Ironically, there’s a reason we did this in February. And so now this is sort of just my new thing as you have to talk about it, you have to get it out there.
So I try every month to put a post on my little Facebook group and in our eagle support groups about my healing, what we’re doing, please share this, talk about it, and I talk to patients, Dr. Hackman’s patients, he’s like, “I get tired of hearing your name before I go into the OR” because people, I’m like, “tell ’em I said hi.” But I talk to them before surgery, because everybody’s always, it’s terrifying, because you’re so sick and dying, and like you said, I’m really lucky.
There’s patients around the world who go through dozens of doctors like Nora Sophie, who, oh God, it hurts my heart to think of what that girl went through. But once you find someone to treat you, the healing is almost as hard as the illness.
And so think of it like if you had chemo and radiation and stage four cancer and you were recovering, it’s like that, but again, how you heal is completely different from just about anything you’ve ever done before. So if she was brave enough to get up and talk, and I’ll have to send you a link for her.
It’s amazing, amazing to listen to her. And she just published her first book of poetry that she wrote about her illness and being sick and being in hospitals and she’s just a beautiful soul. And she started talking because she wanted to raise awareness for eagle syndrome and rare diseases. She said she inspired me.
Emily: That is amazing. And it’s just, yeah, like you said, there’s not really anybody to teach you how to heal. And if you can come in there and provide that support for people, and like you said, just talk to ’em before surgery, alleviate that anxiety, like what a beautiful gift that you can give people now that you’ve been on the other side and sort of been through this and now I can help you through that. That is so sweet.
Annie: Right? Aw, thank you. Yeah, it’s amazing ’cause I try to tell them, people are always so fearful and it’s normal. It’s normal to think worst case scenario, I’m going to have this, this could go wrong, this could go wrong, but what if you think the best? What if you imagine the best that could happen?
I mean, my outcome, sure, maybe in a million years I dreamt about this, but I never thought I would have this go good of an outcome, and so my surgery had not been scheduled until March and then they opened up the ORs February 14th and I was at the top of their list.
So they called and said, “can you be here Wednesday for surgery? You need your COVID test, you need,” I’m like, “I’m there.” My bag’s been packed for months. And so, oh God, what was it? Oh my gosh. Oh, so as I’m getting ready to go, we’re in the car, grabbed my iPad and I type my goal list, right? What I hoped would resolve and feel better after surgery. Not every symptom, but maybe 15, 16 of them.
And so getting ready to go into surgery, I’m all prepped and stuff and Dr. Hackman pops in and he is like, “all right, I’ll see you.” I’m like, “no, no, no. Come here. You need to read my goal list.” And I literally, again ’cause I’m that patient, hand him my iPad and he is like, “great, okay, I’ll see you inside,” right?
And so my one month follow up with him, I saw him after surgery but then did not talk to him until one month after. And so we get on the phone and you can hear him, we weren’t on a video, we were on a call, and you can hear him sort of doing things and he’s like, “how’s everything?”
Blah blah working, working, “and how are your symptoms?” And and I’m like, “well, you’re going to be surprised to hear this.” And he is like, “yeah, huh huh.” And I’m like, “32 of the 33 symptoms I have resolved.”
And it was just like, he just froze. You could hear everything stopped and he is like, “wait, what did you say?” And, I said, “32 of the 33 symptoms resolved.” And he said, and he was just done. He said, “oh my gosh.” He said, “I thought as sick as you were, you would be lucky to have six or seven symptoms resolved.”
And so we chatted for a minute and he goes, you know, he goes, “I owe you an apology.” He said, “because when you showed me your goal list,” he said, “I thought it was a little optimistic.” And he said, “it just goes to show you the power of positive thinking and just what the mind can do.” He said, “we really know so very little about it,” so.
Emily: Oh my gosh, that is such a good story.
Annie: Right?
Emily: I feel like it fits into what you’re kind of might be doing here in the future in showing other people that if they really believe, if they’re positive, if they keep that mindset that they can have an outcome as amazing as yours.
Annie: Yeah, yeah. It’s not perfect. My face is not going to look like it did before. I may have some of the nerve sensation forever, but it’s not painful, and I’m alive and I’m here and I’m engaged in life and, you know, having my furniture delivered. Finally, after two and a half years in a new house, we’re finally finishing up unpacking boxes and moving in.
Emily: Oh my gosh, you have your life back.
Annie: I really do. Like happy anniversary, right?
Emily: I know! In just a year or two, I know a lot of people are like, “oh, it’s a year,” but when you were living like you were living and to see you as well as you are now in just a year, like, my god.
Annie: It’s hard to wrap my head around sometimes. I try not to think too hard about it, because yeah, it’s a lot. And you just got to keep moving forward every day. Even if it’s one little thing. I used to say I did three things a day and some days I would wash my face and brush my teeth and maybe put clean pajamas on. But that was three things. So yeah, it doesn’t matter how big they are, they’re three.
Emily: Just getting ’em done! Absolutely! And now today you can do as many things as you want to do or as little as you want to do, and that is so beautiful, and really a story of hope for so many people listening.
A lot of people are living how you were living and to see the improvement, the changes that can be made, I just am so thankful that you’ve shared all of this with us today because it’s just inspiration.
Annie: Oh, it’s my pleasure.
Emily: I feel like, yeah, like, “oh my gosh!” I’m just so happy for you, Annie, truly.
Annie: Thank you. I am too! I mean it hurts, ’cause I suffered for so many years and I’m not the only one. There are so many who suffer because their doctors don’t listen to them and you really do, you have to be your own best advocate.
And I went to, I saw this doctor at the UVA, at University of Virginia UVA, and you know, I don’t mean this literally, but I’d still like to punch her in the nose if I saw her again because she, when I saw her, basically said to me, “there’s no way any of this is related to Eagle syndrome” and completely blew it off that, you know, “it’s all in your mind, you’re just,” blah blah blah, blah.
Anyways, as I left there, I was just crushed. Crushed. And one of my friends said to me, the best, best thing Kimmy said to me was, “she wasn’t the one for you. Move on to the next doctor.” And it was that simple that it’s like, you know what?
Don’t give that doctor that much space in my head. Move on. Keep looking. And it was shortly after that that I found Dr. Hackman. So yeah, but yeah, everybody, they all have journeys like that. I mean, and some of them live in states where their insurance doesn’t allow them to go out of state to a doctor or, you know, and again, then you’re in long-term pain management, care management, you know? Full circle back to what do you do to take care of that? How do you manage it?
Emily: Oh my gosh. Just being your own health and wellness advocate I feel like is one of the most important things that we can learn, and it’s hard to learn, but you have to do it because like you said, in healthcare, if you get stuck with the wrong doctor and don’t choose a different doctor, your fate is sealed.
And I feel like a lot of people feel like they’re stuck with their doctors. But I always tell people like, you’re the customer, you can change doctors.
Annie: Oh gosh, no. Oh yeah. Do you know the same said female, one of the reasons I wanted to punch her in the nose was because at one point she said to me, “don’t feel like it would offend me if you went to get a second opinion about this.”
And I wanted to say, “when the heck makes you think I need your permission to get a second opinion?” At that point I was done with her. At that point it was just like, yeah, move on.
Okay, yeah. Almost makes it easier to be like, “yeah, not the one for me.” But I will say how I found you Emily, is as I was reading, because I didn’t need prescription medication anymore, I stayed on the Gabapentin for almost two months after surgery because that helped the nerves and with all the nerve healing, it kept the sensation down.
But I tapered off of that by I think mid-April, the end of April, almost two months after surgery. But as I was looking for different products and how I got to your page, I wanted legitimate information about the products.
Like, you know, I’m in Virginia, so you could get your medical, and only in July they were backed up years and years getting your medical card. I mean like five or six years. It’s ridiculous. And so they finally, like July 1st, I believe it was, right? July last summer?
Pass a law where you can get your medical certificate, you don’t have to have a card now, you can just use your certificate in the state of Virginia. You can still apply for your card and wait, but it’s still a years long wait for a card.
And so because as I’m reading, it’s like what, how do you know the difference between Delta-8, Delta-9, and Delta-10? How do you know if you buy this product from this company online? You know, weather, and I think my brother-in-law had given me the product, the nighttime one that I was using.
But I like your page, I kept coming back to, because I like that you have the third party lab testing. I like that you can go back through your batch numbers and read about how they were tested, what was in it, what the percentage of it is.
I like the consistency of it, and I like that you explain really in depth, like you do go down the rabbit holes and that’s a good thing sometimes. But I’ve learned probably the most I know about it from you, so yeah.
Emily: Oh my god, I’m so glad that you found me and it really, it just to even play a little role in your healing journey and getting you to feel this much better, like it makes everything I do worth it. It makes me so happy for you.
Annie: Yeah. Yeah. Well thank you. I love the oil, the butter, your two new like cooking products, like for me that like, it’s a slower gentler release and as I deal with this nerve stuff, it’s just a very low, I don’t know, it’s hard to explain it, but it just sort of just calms it without putting you to sleep or without, you know, putting you in couch lock or whatever. Which I know I’m not that client.
Emily: Oh my gosh, I’m so glad that you’ve been experimenting with new things too and finding what works for you and I should say thank you so much for being such a supportive customer.
It just makes me feel so good to know that these products are actually helping real people, like to see you here and have you tell me like it works, it’s helping me, just makes everything that I do feel worth it, and so I can’t thank you enough for telling me. It really means the world.
Emily: Oh you’re welcome. Oh, when you said that your, they canceled your and I’m just stunned, because I’ve seen stuff. I have a friend’s son who is a videographer in California and works for cannabis companies.
He produces videos for them and they are on his Instagram thing 24/7 and I’m going, well, he puts on with him and his friends and stuff is nothing like what you put up. So I’m like, “how can she be shut down and he not be?” Again, it’s just-
Emily: It’s so crazy, you know-
Annie: It does not make sense.
IEmily: just believe everything happens for a reason and I’m glad that the universe made that decision for me because ultimately-
Annie: I like that you think that way, because when the door opens or when a door closes, a window opens.
Emily: Now, I will say I had a pity party for like two weeks. I was super sad about it, but now looking back on it, I’m here talking to you because that happened.
And it just makes me feel, again, everything happens for a reason and I know that’s not easy to hear if anyone’s listening in pain and not feeling well today. But I do think that we’re all on this journey and it leads us to where we’re supposed to be. And like just to be here talking to you and have this conversation just feels so full circle and so special.
I really thank you for being so open and honest and sharing your story. And I want to be respectful of your time, but I also have four questions for you.
Annie: Oh, sure!
Emily: Are you ready for them?
Annie: I love a good question.
Emily: Awesome. Okay, so the first one is, what are you most proud of in your life?
Annie: I am most proud of my beautiful children and my husband. February 6th, we had our 41st wedding anniversary.
Emily: Oh my gosh, congratulations!
Annie: Yeah, he’s amazing. Yeah, I could not have gotten through this without him. So yeah, my family, my husband and my kids are the best thing in my life. I love them.
Emily: They have to be so happy to see how well you’re doing it.
Annie: Yeah, yeah. I could not have gotten through this without them, that’s for sure.
Emily: I bet. Oh my gosh, 41 years. Congratulations.
Annie: Thank you.
Emily: That’s amazing. So this is everybody’s least favorite question. What do you think your life would look like without cannabis?
Emily: I think it would be really chaotic and frenetic, this healing. And I’ll tell you why. Because I don’t, again, Valium, Xanax, that kind of stuff has almost the opposite effect on me. In 2011, I had a lumpectomy and when they sent me in for the breast biopsy, they do the wire insert and it’s ugh.
Anyways, they gave me a Valium, I’d never taken it, but that way they explained this to me, you’re going to need this before you go in. So I took it, right? And I’m telling you, to this day, it was like a horror nightmare, terror. It made me so agitated. I mean, I remember screaming at my husband in the car because I didn’t like the route he drove to the hospital and he was just driving around traffic.
He was doing nothing wrong. By the time I got in there, I was sobbing. It has a complete opposite effect on me! So I don’t know what my other option would’ve been. There would’ve been nothing else I would’ve gone to. So I can’t imagine being like, “ah.” That’s what it would’ve been like.
Emily: Just to have that like calmness is such a gift.
Annie: Right. As soon as we’re done talking, I’ll go, ’cause I can already, like-
Emily: You were telling, I know it’s probably hard for you to talk a long time, so I’m going to wrap this up.
Annie: But I didn’t lose my voice, so that was good.
Emily: You sound amazing, yes. Second to last question, if you could go back 10, 20, 30 years ago and give yourself a piece of advice cannabis related or not, what would it be?
Annie: So I’m going to give you three answers. 30 years ago I would’ve said, it’s not your fault. It wasn’t your fault. 20 years ago, I would’ve said keep doing what you’re doing because life is awesome. 10 years ago I would’ve said, “you are not going to believe what’s down the road.”
Emily: Oh my gosh. I love that. That is so perfect. Last but not least, if you could be remembered for one thing in life or in the cannabis space in general, what would it be?
Annie: Happy, joyful. I’ve been accused of being happy, too happy, more than once in my life. And like if that’s the worst thing you can say about me, bring it on! But yeah, you said it a little while ago. There is always hope.
There is always something to hope for. Always. And man, I’m telling you, I was weeks away from dying and I didn’t. and so it just goes to show you, think positive, hope for the best. Don’t expect the worst. Hope for the best, man. Think about that. It changes everything when you think that way.
Emily: Thanks so much for sharing that. Like my hope is that someone on the other end is going to listen to this, who maybe was in the situation you were in, and to see how far you’ve come, and to give them that hope.
And you’re sharing your happiness and joy with us here. I can’t thank you enough, Annie! I enjoyed this conversation so much.
Annie: Oh good, me too!
Emily: So happy for you to see the progress you’ve made.
Annie: Thank you. You’re a joy! You have a beautiful light too. You have a beautiful light around you.
Emily: Thank you so much. This is so special.
Annie: Thank you for what you do. I couldn’t, I would not be where I am without the little bit of help from you too, so thank you.
Announcer: Congratulations, you’ve finished another episode of the Well With Cannabis Podcast and are one step closer to discovering how you, too, can live well with cannabis.
Thank you for listening in today. We hope this episode has been a helpful and informative one. Please visit emilykylenutrition.com for more information on today’s show, show notes, guest information, recipes, and other resources.
If you want more support and encouragement on your cannabis journey, please consider joining the private Well With Cannabis Community. In this group, you can connect with like-minded individuals focused on improving their health and wellness through cannabis.
Join the group today to continue your journey of wellness together!
Stay Connected